Immune System & Allergies
Our Immune System
Nature has provided us with a sophisticated defense system against diseases. Over the course of evolution, it has had to constantly "update" itself and develop new defense strategies to protect us from pathogens. We can think of the immune system as a kind of "family business" in which everyone has their own job. If not faced with an imminent attack on the immune system, then the immune cells can laze around. However, if a microbial enemy approaches, then the immune system knows what to do to protect the system: pull together is the motto!
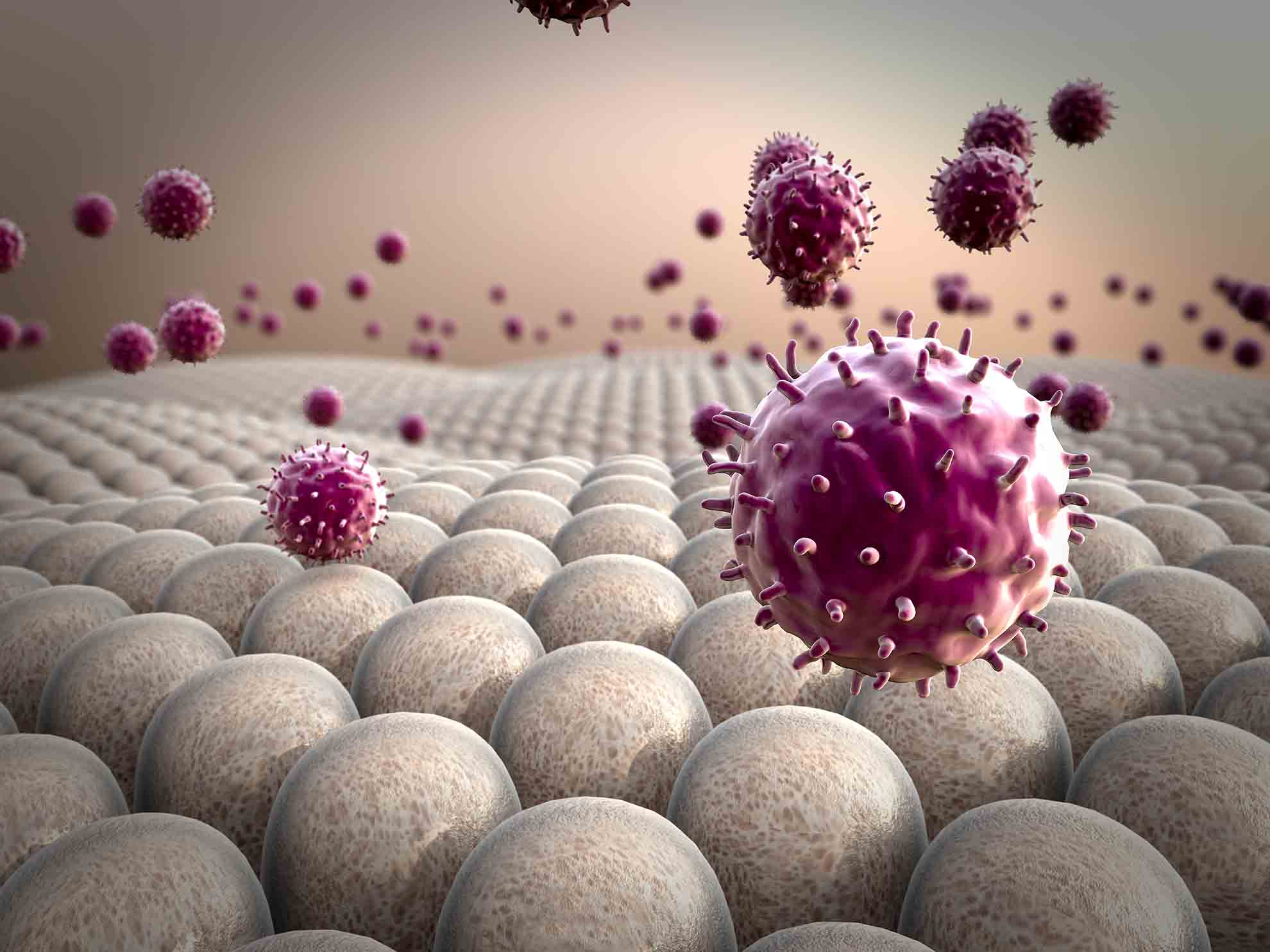
The bacteria in the uppermost layer, i.e. on the skin or on the mucous membranes, are the first barriers that an intruder must first overcome. If there are enough good bacteria, then it is easy to get rid of the troublemaker. However, if the pathogen manages to outwit the first hurdle – whether through camouflage or deception – then it faces the next level, where the intruder may be expelled - or not. For our immune system, this means that when pathogens reach the mucous membrane of the digestive tract, e.g. in the mouth, intestines or stomach, enzymes ensure the defense of the healthy system and cilia and epithelial cells ensure the removal of the enemy. The systemic interaction of countless lone fighters – as in a well-coordinated team - ensures a successful immune defense in our body.
In the immune system, leukocytes, better known as white blood cells, play an essential role in the initial defense against pathogenic germs. Leukocytes have a great "kinship", for example, neutrophilic granulocytes have the special property of recognising the enemy attacker and saving its profile. T- and B-lymphocytes have very special sensors, they are called antigen receptors, in order to scout out and kill the enemy, for example, an unknown protein.
Fortunately, lymphocytes, also known as "memory cells", remember this for a lifetime. The penetration of unknown proteins is "reported" with the help of the dendritic cells. T cells then release cytokines (messenger substances), which initiate the destruction of the enemy. The family of white blood cells also includes monocytes, they turn into macrophages (scavenger cells) if in danger, and decompose the enemy into its protein components. These, in turn, are recognised by B and T cells. If this intruder approaches again after days, weeks, years, B-lymphocytes are called on the scene and the rapid production of antibodies begins, the enemy (the antigen) is eliminated.

Our Defence Mechanism
The place where our system defends against these enemies is in the lymph nodes of the lymphatic system, such as found on the neck, in the armpits, in the groin or in the abdominal area, where B and T lymphocytes are located. Their accomplices are dendritic cells that "convict" the enemy so that it can be destroyed. For this, immunoglobulins (protein antibodies) are formed by the B cells, which are specifically directed at the enemy and destroy it. In the infection phase, immunoglobulin M (IgM) and immunoglobulin G (IgG) are typically formed in the blood even after weeks of infection. On the basis of IgG, it is therefore also possible to detect a survived infection in the blood.
But how do the defenders know where they are needed? The messenger cytokines and chemokines are responsible for this. Cytokines signal where the infected tissue is located, and chemokines direct the defenders there. Inflammatory processes occur in the body by causing redness, warmth or swelling in the affected area. There is, however, a reason for this, namely, to accelerate the defence process by indicating the affected area.
"The majority of antigens enter our body through the intestines – that is, through food. “
Children & their Immune System
It is not only the genes that parents pass on to their offspring that determine how a child develops. Already even when in the womb, the immune system of the embryo is shaped, because the mother's blood also encounters antibodies for various pathogens.
The mother's intestinal flora also has an impact on how the child's defences develop. There are studies that clearly show that the bacteria in the mother's intestines contribute to forming the baby's immune system. If the mother takes beneficial bacteria in the form of probiotics during the last month of pregnancy and if this treatment is continued in the baby during the first six months of life, then these children are less likely to develop neurodermatitis later.

Allergies
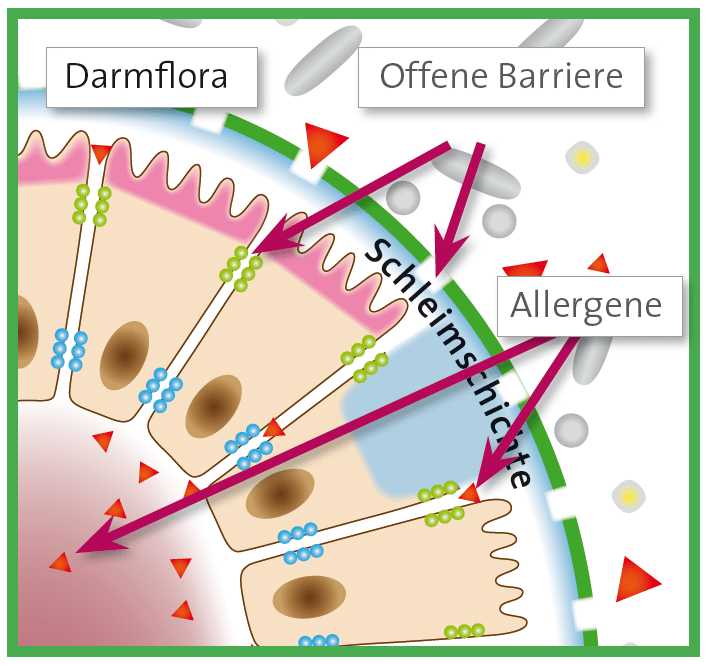
Allergies can arise when the mucous membranes in the body (nose, lungs, intestines) are damaged. In this case, the substances entering the body with the air or food are not properly controlled or classed as harmless but immediately and uncontrollably get into the blood or lymphatic ducts. This uncontrolled excess can lead to an overshooting of the immune system: allergies and food intolerances are the consequence.
Allergic Reactions
Despite various symptoms of allergy, the course of all allergy reactions is the same: upon contact with allergens, antibodies to this allergen (lgE) are formed. Upon renewed allergen contact, these IgE antibodies mediate the release of histamine, which triggers the typical allergy symptoms: e.g. itching, watery eyes, swelling, rashes or asthma. When this allergic reaction takes place, the allergen has been able to pass the first barrier of the intestinal mucosa undetected.
In the intestinal mucosa there is a special antibody, the sIgA, which normally prevents the penetration of harmful substances and allergens. sIgA is formed by the cells of the intestine and secreted into the mucous layer. As a "mucosal antibody", this antibody is a kind of protective coating of the intestine. It protects us against allergies as the antibody attaches itself to unknown substances even before they are absorbed into the body and marks them. If allergens have been labelled in this way, they can no longer be absorbed by the body. This will prevent an allergic reaction before it can arise.
Allergy Protection = Protect Mucous Membranes
The principle of mucosal protection is a basic concept for allergy prevention. After all, this way any substance that triggers an allergy is repelled. Whether this substance comes from plants or animals (e.g. grass pollen, animal hair), from food (e.g. preservatives, flavors), or from care products is not a decisive factor here. Therefore, it is possible to treat several different allergies by means of treating the intestinal mucosa.
What can you do about allergies?
Nowadays, allergies can be treated in various ways. In symptom-oriented treatment, the effects of allergy are treated. The symptoms can be "stopped" for a short time by drops, sprays and tablets to decongest and reduce histamine release, but the causes of the allergy are not treated by these measures. Another way is desensitization: the body is gradually accustomed to a certain substance that triggers the allergy and therefore builds up tolerance to the substance. This way is suitable for allergies to individual known substances, but it is lengthy and does not protect against new allergies.
The long-term convincing way is by treating the mucous membranes. These are not intact in allergy sufferers and are causally involved in the development of allergies. Treating mucous membranes targets the origin of the allergy and is especially indicated for people who are allergic or intolerant to several substances.
Children & Allergies
What factors promote the development of an allergy in childhood? How can parents reduce their offspring's risk of developing the disease? And: How does a pollen allergy actually manifest itself?
Respiratory allergies are steadily increasing in children and adolescents. An important role in the development of not only annoying but enormously burdensome hay fever is played by hereditary predisposition. If one or even both parents suffer from an allergy, then the child is also likely to be affected with a high probability. In addition, babies who are born by caesarean section and therefore do not come into contact with the maternal intestinal flora are more at risk.