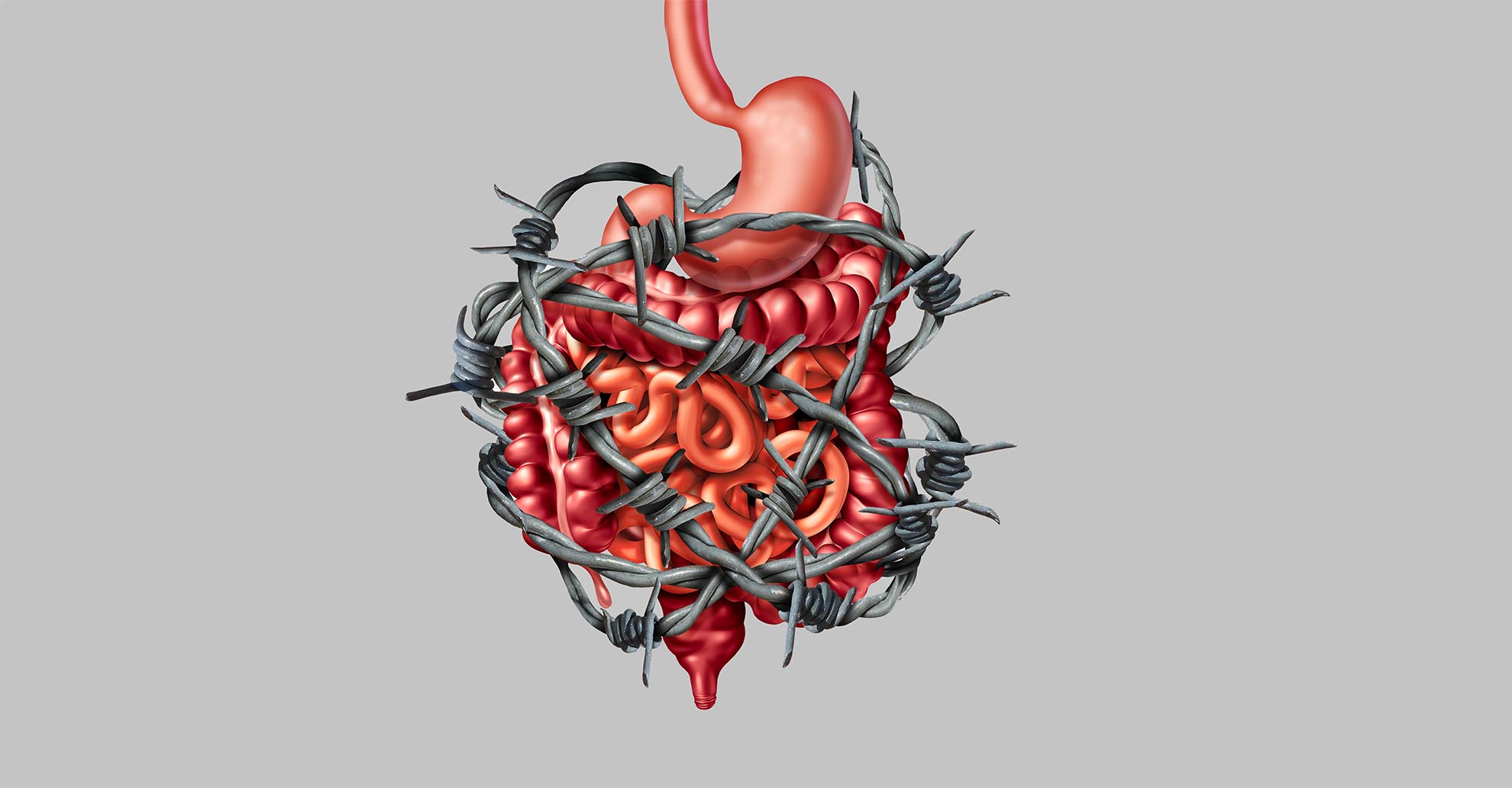
Irritable bowel syndrom - IBS
In irritable bowel syndrome, the patient has various symptoms in the gastrointestinal area - but without organic causes. It is a functional disorder of the digestive system. Read more about who can be affected and the possibilities for diagnosis and treatment here.
What is the irritable bowel syndrom (IBS)?
Irritable bowel syndrome (IBS) is one of the most common functional disorders of the gastrointestinal tract. Not only the colon is affected, but the whole digestive system is affected. Despite thorough medical examination, no organic cause can be found for the often-severe digestive problems. It is estimated that about 20 % of the population in industrialised countries suffer from irritable bowel syndrome to a greater or lesser degree. Women are affected about twice as often as men. The symptoms usually appear for the first time between the ages of 20 and 30 and often last for months or years. Often, the use of antibiotics in connection with an intestinal infection can also be identified as a trigger (the so-called post-infectious irritable bowel syndrome). The quality of life for people who suffer with IBS is often considerably reduced.
Which symptoms occur with IBS?
Typical symptoms of irritable bowel syndrome are abdominal pain, cramps in the abdomen, flatulence, constipation and/or diarrhoea. Stress additionally aggravates the symptoms. The symptoms sometimes disappear after a bowel movement or occur more frequently after eating, especially if too much has been eaten. Then it may be that the digestive enzymes are not sufficient, and putrefaction and fermentation dyspepsia occur, which in turn triggers flatulence. Sometimes there is a feeling as if the bowels cannot be emptied properly. Heartburn, belching and bowel sounds may also occur. Only after other serious diseases have been ruled out (other causes for the symptoms must be excluded), can the diagnosis of irritable bowel syndrome be made. The disease itself is very distressing, but not dangerous.
Complaints of irritable bowel syndrome
Irritable bowel syndrome (IBS) may be diagnosed when the following 3 points are fulfilled:
- You have chronic symptoms, i.e., lasting longer than 3 months (e.g., abdominal pain, flatulence), which are usually accompanied by changes in bowel movements (diarrhoea, constipation or alternation between diarrhoea and constipation).
- The symptoms are the reason why the patient seeks help and/or worries a lot and the symptoms must be so severe that the quality of life is relevantly affected.
- The prerequisite is that there are no changes that would indicate that the patient is suffering from any other condition.
Accompanying issues
Patients suffering from irritable bowel syndrome often also have the following problems or complaints:
- Anxiety disorders
- Depression
- Insomnia
- Chronic fatigue syndrome (CFS)
- Headache (migraine)
- Fibromyalgia (so-called "soft tissue rheumatism with diffuse pain symptoms)
- Menstrual cramps
Irritable bowel syndrome
A meal with friends, a concert, or a trip - what many people can enjoy without a second thought is denied to sufferers of irritable bowel syndrome. When the gut rebels, there is no longer any question of quality of life. However, special probiotics can address the cause of these problems.

What can cause irritable bowel syndrome?
In people with irritable bowel syndrome, food passes through the digestive tract either too quickly or too slowly. Affected people can therefore suffer from diarrhoea (passage time too fast so that no fluid reabsorption can take place, the stool remains thin) or constipation (passage too slow). Often there is an imbalance in the colonisation of the gut (the normal intestinal bacteria that help with digestion are in the minority, harmful, gas-forming bacteria gain the upper hand), more intestinal gas is formed, which leads to bloating, flatulence, and severe abdominal pain. In addition, the sensitivity to pain is increased in irritable bowel patients due to, among other things, a lowered pain threshold to stimuli. The intestinal barrier protecting against harmful substances is weakened, the intestinal wall becomes more permeable ("leaky gut"): meaning that harmful substances cannot adequately be removed. Stress also aggravates the symptoms. Patients with irritable bowel syndrome have an increased susceptibility to depression and anxiety disorders. A dysfunction of the autonomic nervous system together with psychosomatic disorders is often mentioned here.
Triggers of irritable bowel syndrome
There are various theories about the medical causes of IBS. Among other things, bacterial infections of the gastrointestinal tract, a disturbance of the immune function in the digestive system and an abnormal intestinal peristalsis (motility disorder) are assumed to be the triggers of IBS. Scientists have been able to identify a whole series of typical changes in the intestines of those affected. However, these changes do not only occur in irritable bowel syndrome, but also in chronic inflammatory bowel diseases, diverticulitis, and food intolerances.
Serotonin production imbalance
The messenger substance serotonin is also responsible for how pain is perceived. If the nervous system of the bowels is stimulated by IBS, it can no longer correctly regulate how much messenger substances are produced. It can then happen that patients feel their bowels more strongly and experience pain, whereby among ‘healthy’ people these stimuli do not exceed the threshold of perception.
Disturbed bowel motility (the ability of the intestines to move)
The intestinal wall of IBS patients reacts highly sensitively to stretching stimuli created by food. The bowels possess their own nervous system in the intestinal wall (the enteric nervous system, ENS), sometimes referred to as the brain of the abdomen. It signalises when food has reached the bowels and is stretching the wall. Together with the messenger substance serotonin, ENS controls digestion by stimulating the bowel muscles to tense and relax alternately, thus created a peristaltic wave and moving the food forwards. In IBS this intestinal nervous system is disrupted and irritated – it issue erroneous instructions to the bowel muscles. This leads to unsynchronised bowel movements and digestion is thus impaired overall. The chyme or food pulp is either moved too quickly leading to diarrhoea (irritable bowel syndrome with diarrhoea), or the opposite happens: if the muscles move too slowly, constipation can arise (irritable bowel syndrome with constipation). Irritable bowel cramps and flatulence occur when the muscles contract too strongly and no longer relax completely.
Infections of the gastrointestinal tract as the cause of IBS (post-infectious IBS)
Several studies have confirmed that an irritable bowel can be a consequence of gastrointestinal infections (so-called stomach bugs). Bowel infections with specific bacteria (such as Campylobacter jejuni, Clostridum dificile and harmful E.coli) tend to cause irritable bowel more than other pathogens. An enteric (affecting the bowels) infection is, however, only responsible for one in ten cases. If a bowel infection is the cause of IBS, patients typically develop characteristic diarrhoea symptoms. Antibiotics – which are often too hastily deployed against bowel infections – also damage the intestinal biotope and can trigger an irritable bowel.
Increased immune activity in the intestinal mucosa
In tissue samples of the intestinal mucosa of those affected, increased immune activity can be established. An increased number of immune cells and their messenger substances (inflammation mediators such as interleukin) can be detected in the mucosa. Where this increased reactions come from in IBS and what they are possibly good for is still being intensively researched
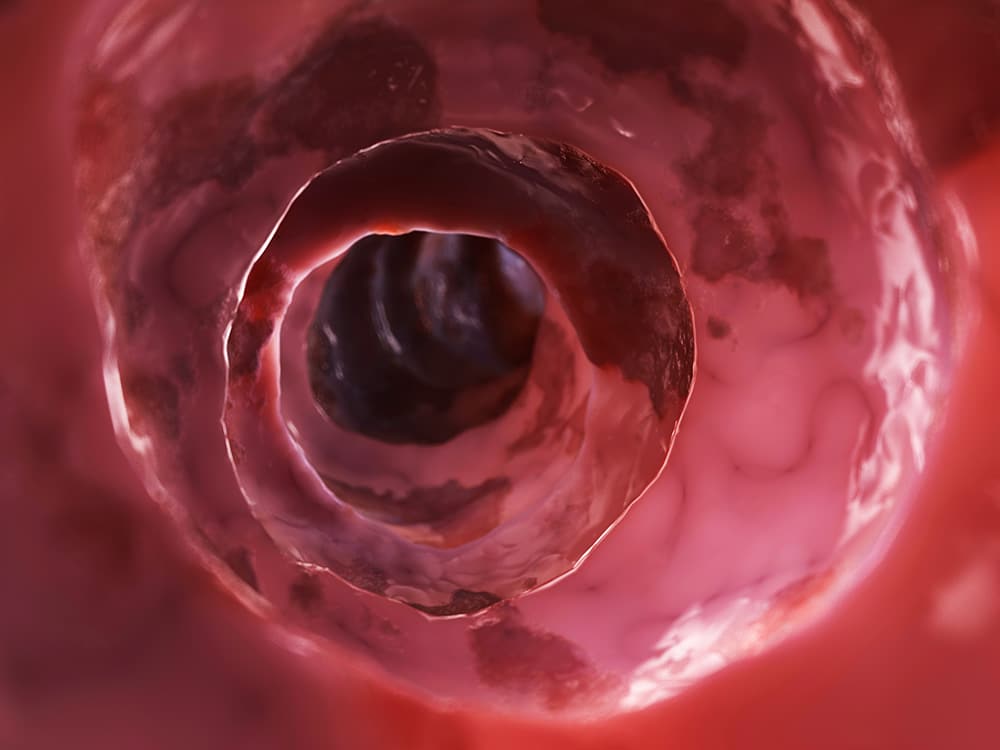
Increased permeability of the bowel mucosa („Leaky Gut“)
In the intestinal mucosa, neighbouring cells are connected by so-called tight junctions. They seal the cells in relation to others so that no foreign substances or pathogens can move between the cells. As long as this barrier is intact, the totality of the intestinal mucosa cells form a protective shield preventing the intrusion of external substances from the bowels into the body. In IBS, this barrier is leaky or ‘holey’, i.e. the cells are no longer so tightly connected, pathogens and toxins can penetrate the mucosa more easily, leading to an immune reaction – inflammation.
How can irritable bowel syndrome be diagnosed?
The diagnosis of irritable bowel syndrome is made based on the typical pattern of symptoms and after ruling out other conditions.
- Where do you have pain and in which situations does it occur?
- Do you have diarrhoea or constipation?
- Have you noticed a connection between the pain and certain foods or drinks?
- Do you have other symptoms such as vomiting, muscle and joint pain, heartburn, and fever? Have you noticed blood in the stool? Do you feel tired quickly? Have you lost weight? This would be atypical for irritable bowel syndrome and is considered an alarm sign to look for serious illnesses.
- Are you experiencing high levels of stress?
- Do you have any other conditions? Ask about triggers and circumstances (e.g., stress, anger, overwork) that aggravate the complaints.
- Do you regularly take medication, or have you done so in the last few weeks (including antibiotics, painkillers, heart medication, thyroid medication, and laxatives)?
- Questions about family history (health conditions in the family)
- Presence of organic bowel diseases (e.g., chronic inflammatory bowel disease (IBD) associated with severe diarrhoea).
Before diagnosis, the doctor will conduct a full health analysis.
How do you recognise irritable bowel syndrome?
After this conversation, a physical examination takes place, during which the doctor may look at the anus and may press and listen to the abdomen. A stool sample can also provide information about digestive disorders and functional malfunctions of the intestine. The stool is examined for hidden (occult = not visible) blood. In addition to the intestinal tract, the doctor also checks the urinary bladder, the kidneys, in women the ovaries and, depending on the symptoms, the heart. An analysis of the blood and stool (blood in the stool, parasites (worms)), the urine as well as functional tests of the organs also provide important information. Like with bloating, food intolerances such as fructose, lactose, sorbitol intolerance, etc. must be ruled out. If the symptoms are acute, accompanied by weight loss, fever, fatigue, anaemia, vomiting, joint complaints and/or blood in the stool, they may be caused by another serious condition and further medical clarification of the underlying disease is necessary. Liver problems, gall bladder or pancreas diseases must be investigated.
This may be followed by an examination of the rectum and the large intestine (colonoscopy). During a colonoscopy, the large intestine and the end of the small intestine are examined endoscopically through the anal canal. The intestine can also be visualised on an X-ray using a contrast medium. If an organic disease, food intolerance or chronic inflammatory bowel disease has been ruled out, the doctor will diagnose irritable bowel syndrome. Irritable bowel is a "diagnosis of exclusion", which can only be diagnosed when all other causes have been ruled out.
Other possible diagnostic measures:
- Ultrasound examination of the entire abdominal cavity (sonography)
- X-ray examination of the intestine and abdomen (X-ray), today mostly in the form of computer tomography (CT).
How can irritable bowel syndrome be treated?
Irritable bowel syndrome is an unpleasant condition that strongly affects the quality of life. Medical treatment is only possible to a limited extent and is symptom oriented. The most important thing is first to be able to classify your symptoms and not to worry that there is a serious illness behind them. Since the side effects of conventional medicines can often be severe, it must be weighed up whether the risks of the medicinal treatment are not greater than the symptoms themselves.
Often, a change in diet and the avoidance of foods that cause flatulence and are difficult to digest can relieve the symptoms. Natural remedies can be sufficient as the sole therapy for mild symptoms, but they can also be used to support conventional medical treatment.
Peppermint oil in gastric acid-safe form, whose active ingredient is released in the small intestine, has a relaxing effect. Chamomile, lavender oil, coriander, lemon balm and calamus also have a calming effect on the stomach and intestines. The plants mentioned are available in tea preparations and ready-to-use preparations at the pharmacy, for example. Special organically produced preparations made from papaya fruit counteract complaints such as flatulence, pain during bowel movements or constipation and calm the digestive system, which is in a state of alarm.
If stools are very hard, carefully tolerated high-fibre food can be tried. Caution is advised, as dietary fibre can also cause flatulence. Mucilages such as linseed, Indian psyllium and wheat bran promote intestinal transit in constipation, absorb a lot of water and reduce diarrhoea. Foods such as rice, potatoes and oats have a constipating effect. For flatulence, caraway, fennel and aniseed preparations or teas provide relief.
What helps with irritable bowel syndrome?
Recent studies indicate that irritable bowel syndrome is also associated with mild (chronic) inflammation and a less diverse, functional bacterial flora in the intestine. Irritable bowel syndrome often occurs after intestinal infections, especially often when these are treated with antibiotics, as this additionally destroys the natural, healthy intestinal flora and the harmful bacteria can continue to spread unchecked - the result is an increasingly "permeable" intestine, the protective barrier of the intestine is destroyed. Myrrh, camomile, and coffee charcoal have a sealing effect on the intestine.
Probiotics for irritable bowel syndrome
However, to effectively counteract the many causes of IBS, there are gentle methods that combat the causes of IBS and prevent IBS symptoms. Natural intestinal bacteria or probiotic bacterial preparations are recommended by medical-scientific committees and associations for all IBS symptoms. These probiotic intestinal bacteria not only eliminate the symptoms, but also the causes of irritable bowel syndrome and restore the balance in the intestine in three ways:
- Intestinal bacteria are completely natural microorganisms that occur in the healthy intestine and support our digestion and well-being in many ways.
- Intestinal bacteria have no unwanted effects - occasionally, when you start taking a bacterial preparation, there may be slight flatulence and stool changes. However, this is temporary before the beneficial effects begin.
- With intestinal bacteria (including bifidobacteria, lactobacilli, lactococci, streptococci) - which are combined in special compositions against the various causes of inflammation, "leaky gut", harmful germs (often after antibiotic treatment or intestinal infections), motility disorders. The causes of the symptoms are addressed and eliminated.

The regular intake of probiotics helps to strengthen the intestinal mucosa and its barrier function and to prevent or stop inflammatory processes.
For scientist Christoph Högenauer, this approach is exactly in line with previous study findings. The expert: "A recently published meta-analysis of 35 relevant studies shows that not all probiotics are equally effective - but depending on the symptom and problem, they have an extremely positive effect overall. Multispecies probiotics seem to work better than monostrain probiotics in most studies to relieve distressing symptoms." For example, the summary of all studies shows an improvement of the typical symptoms in 21 per cent of those affected, 25 per cent had less abdominal pain and bloating; the frequency of the dreaded urge to use the toilet could also be significantly reduced.
A new paper from the Medical University of Graz has focused on the effect of probiotics in irritable bowel syndrome. The focus was on the immune system of the intestinal mucosa (also called the mucosal immune system) and how anti-inflammatory bacterial strains support the intestine to regulate stress-related disorders. The result: Regular intake of this synbiotic helps to strengthen the intestinal mucosa and its barrier function as well as to prevent or stop inflammatory processes. The happiness messenger serotonin and the sleep hormone melatonin can be sufficiently produced again, the gut can then rest. In the meantime, the German Society for Gastroenterology, Digestive and Metabolic Diseases (DGVS) also recommends in its guidelines the use of probiotics for irritable bowel syndrome, whereby the choice of bacterial strain should depend on the symptoms. The DGVS also recommends probiotics for pain, diarrhoea, constipation, and bloating in the course of IBS.
Tips for IBS
Tip 1
Schedule time for relaxation! If you are relaxed, so is your gut! Stress increases the symptoms of IBS. Sufficient relaxation and regular exercise bring the intestines back into balance. Sauna, outdoor exercise are useful. Training in relaxation methods (e.g., autogenic training, yoga) helps to control symptoms of stress, nervousness and anxiety. Patients with severe psychological problems and depression should consult a psychotherapist.
Tip 2
Eliminate gassy and hard-to-digest foods from the diet. This requires creating a food diary and finding out the foods, drinks and situations that influence the symptoms and cause discomfort. Prevention is better than cure. You should avoid irritable bowel triggers! If dietary fibres that stimulate intestinal motility are given, water-soluble dietary fibres (locust bean gum, pectin) should be used.
Many small portions are better than a few large ones! Eat slowly and chew well! Drink enough (e.g., non-carbonated mineral water)! Avoid fatty and flatulent foods as well as very cold and very hot drinks! Carbonated drinks and fruit also often cause discomfort. Eat regularly and always at fixed times!
Tip 3
Smoking should be given up if possible and alcohol should only be consumed in moderation!
Tip 4
Taking probiotic multispecies synbiotics long term that protect the intestinal mucosa and balance the digestive function is ideal for prophylaxis and supportive treatment of IBS.
