
Constipation
Constipation is a problem for many people and sometimes severely restricts their quality of life. Read here about who is affected, how constipation can be identified, and options for diagnosis and treatment.
What is constipation?
Although everyone has bowel movements with different frequencies, constipation refers to having less than 3 bowel movements per week. Generally, a distinction is made between 2 types of constipation:
- acute constipation (also called "situational" or "short-term")
- chronic constipation

Who suffers with constipation?
Around one in four adults in the western world is confronted with the issue of constipation. Increasingly, it is women who have to struggle with constipation, but it is also a relevant and often very stressful and distressing issue for parents and children, even among infants, toddlers, and children. Pregnant women also tend to suffer particularly badly from constipation.
Acute constipation
Short-term (situational) constipation is not a health condition but a symptom, a sign from the body that something is wrong in the body. Medically, constipation can be identified if you have:
- bowel movements occur less than 3 times per week
- this only happens with great effort and pushing and
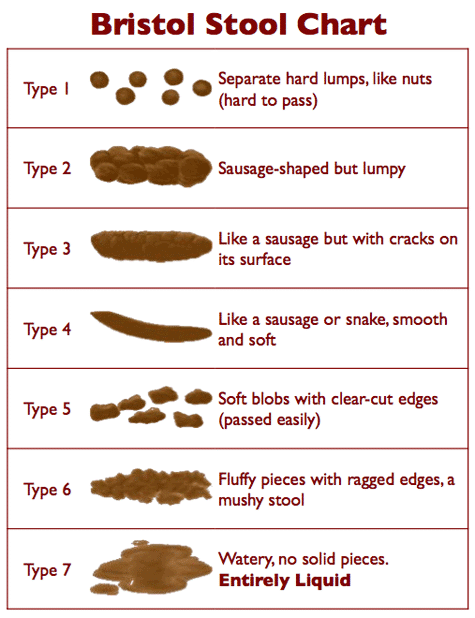
- the stool is hard and lumpy due to the long time it remains in the intestine (see Bristol Stool Shape Scale, type 1 and type 2)
- Additional symptoms often occur outside the intestine
Chronic constipation
Chronic constipation is when symptoms have persisted for at least 3 months and when you experience at least two of the following symptoms in at least every 4th defecation:
- Hard pushing when passing stool
- Lumpy or hard stools (see Bristol Stool Shape Scale, Type 1 and Type 2).
- Feeling of not being able to fully empty your bowels
- Feeling like your bowels are closed
- Using your hand to help pass the stool
- Less than 3 bowel movements per week
- Soft, unformed stools only with laxatives
- Exclusion of irritable bowel syndrome
The difference here lies in the speed of onset and the duration of the blockage.
Acute constipation occurs relatively quickly, i.e., within hours or a few days, whereas chronic constipation develops over a longer period of time - usually more than 6 months.
Constipation is associated with very hard stools, pain during defecation, incomplete defecation, and a feeling of blockage of the bowel. If blood is also found in the stool, if you have severe abdominal pain, fever or constipation and diarrhoea alternate, this is an urgent sign to go to a doctor.
In general, a visit to the doctor is recommended for constipation - especially if it is not situational and short-term.
What can cause constipation?
The causes of constipation can be manifold. It is important to have a general understanding of the physiology of our intestines. This large muscular tube needs a certain volume of stool to receive the necessary "impulses" to transport the contents further. If our diet lacks swelling dietary fibres and the necessary fluid, the required stool volume is missing. If the intake of fluids is too low, the intestine withdraws water from the stool, which makes it hard and difficult for the intestine to transport it further - constipation is then the result.
Other triggers of constipation:
In addition to these causes (such as a low-fibre diet, reduced fluid intake) for constipation, there are several other possible triggers:
- Lack of exercise
- Mental strain/stress
- Physical/organic causes (e.g., pelvic floor changes, haemorrhoids, bowel changes, skin tears in the area of the anus (anal fissures), constrictions in the intestinal tract, etc.).
- Changes in metabolism/hormone balance (e.g., hypothyroidism, diabetes, pregnancy).
- Medicine-related changes (e.g., preparations containing calcium and aluminium for heartburn (antacids), antidepressants, diuretics, medicines for high blood pressure (e.g., beta-blockers), opiates (strong painkillers or the cough medicine codeine), etc.).
- Reduced intestinal motility due to neurological causes (e.g., multiple sclerosis, diabetes mellitus, Parkinson's disease, etc.).
- Disturbances of the electrolyte balance (e.g., potassium deficiency, often also with excessive use of laxatives).
Constipation as a side effect of chemotherapy
People suffering from cancer usually have to undergo chemotherapy or radiotherapy in addition to surgery. Despite the optimisation of this treatment, unpleasant side effects such as constipation or diarrhoea cannot always be avoided. Especially before chemotherapy, the potential benefits of treatment should be compared with the possible side effects.
The cancer itself, but also the treatment used, can cause constipation. However, as these therapies are lifesaving and relieve the discomfort caused by the disease, constipation should not lead to stopping the treatment. People who have always had digestive problems are usually more prone to constipation during chemotherapy. However, acute constipation can affect any patient - regardless of whether or not they have had digestive problems in the past.
Constipation is often caused by long periods of bed rest, lack of exercise and the use of medication. In particular, anaesthetics, drugs against cramps and depression, tranquillisers, painkillers and muscle relaxants have a constipating effect in that they inhibit the natural movement of the bowel. A low-fibre diet, lack of fluids, nervousness and depression can also be reasons for constipation in cancer patients.

How can constipation be diagnosed?
Before diagnosing you with constipation, the doctor will address several points with you.
- Presence of organic intestinal diseases
- Question about other diseases, e.g. neurological disorders (e.g. Parkinson's disease, multiple sclerosis, diabetic nerve disease (neuropathy), etc.).
- Questions about family history (presence of diseases in the family)
- Stool frequency, stool colour and consistency
- Dietary habits - eating and drinking
- Accompanying symptoms such as pain and flatulence
- Ask about medications taken that might have an effect on bowel movements.
- Checking the thyroid function
After taking a medical history, the doctor may perform a physical examination, looking at the anus and palpating or listening to the abdomen. A stool sample can provide information about digestive disorders and bacterial colonisation of the intestine. The stool is also examined for hidden (occult = not visible) blood.
The blood count (thyroid hormones, electrolytes such as sodium, potassium, calcium) is analysed in the laboratory. If these values are within the normal range, if the patient is younger than 50 years and if no warning signs (acute occurrence of constipation, weight loss, blood in the stool, fatigue) could be detected in the medical history, treatment of functional constipation can be started.
In the case of chronic constipation, the examination will be more detailed and a proctoscopy of the rectum and rectosigmoid (procto-rectosigmoidoscopy) may be suggested by the doctor, or a colonoscopy if bowel-related diseases are suspected.
Other possible diagnostic measures:
- Ultrasound examination of the entire abdomen (sonography)
- Radiological examination of the intestine (X-ray), today mostly in the form of computer tomography (CT)
- Determination of the colonic transit time (the time it takes for food to pass through the intestine)
- If an organic cause for constipation is found, the underlying disease must first be treated. If no clear cause for the "constipation" can be found that would allow causal treatment, general measures should first be used to eliminate the constipation.
How can constipation be treated?
The treatment of constipation very often goes hand in hand with a change in lifestyle:
- Dietary changes: High-fibre foods such as wholemeal bread, dates, brown rice, etc. swell the stool and support intestinal activity. It is best to increase the fibre dose slowly, as additional discomfort (flatulence, abdominal pain, bloating) is to be expected at first until the intestines have adjusted.
- Change drinking habits: A glass of water before every meal - this stimulates the bowels. Particularly effective: drink a glass of water in the morning on an empty stomach.
- More exercise: Whether it's cycling, swimming, running or Nordic walking - exercise is one of the keys to success if the bowel activity is to be stimulated again.
- Get in a routine! Bowel training: Do not suppress the urge to defecate! Get the bowels used to regular toilet use again. Daily bowel training brings regularity into the daily routine.
- Colon massage and complementary therapies: A clockwise abdominal massage along the colon stimulates the bowel - five minutes a day is enough. Breathing exercises, yoga, shiatsu, traditional Chinese medicine (TCM), abdominal and pelvic floor strengthening as well as loosening of the leg, buttock and lumbar spine muscles and connective tissue massages (lymph drainage, foot reflexology) can also be used.
- Probiotics: We need various probiotic bacteria in high numbers in our intestines, as they further break down the food in our body and make it usable. If the bacterial flora of the intestine is reduced and damaged (e.g., through medication (antibiotics), stress or an unhealthy diet), fermentation or putrefaction processes begin, which can impair and slow down intestinal activity. To build up and regenerate a damaged intestinal flora, probiotics with highly active bacterial strains are recommended. They protect the intestinal mucosa, promote metabolic processes, and can increase stool frequency, improve stool consistency, and shorten the retention time of food in the intestine.
Home remedies and natural help for constipation
The following home and natural remedies can help with constipation:

- Plums, figs, and other fruit (fresh or dried) as well as sauerkraut (as a vegetable or juice) can stimulate bowel activity. Papaya has a particularly positive effect on constipation symptoms. The digestion-regulating enzymes of papaya increase the mobility of the intestines and harmonise digestive activity.
- Dietary fibres such as linseed, psyllium and bran are bulking and swelling agents that swell by absorbing water (from the intestine); they increase the volume of the food pulp, the intestinal wall is stretched, and the motility of the intestine is stimulated. Sufficient fluid intake is necessary.
- Coffee can also stimulate the reflex to defecate.
- Exercise can be very helpful for constipation! It promotes bowel activity and regular bowel movements if you incorporate exercise into your daily routine.
- Bowel gymnastics - Movement in general stimulates bowel peristalsis. There is one exercise that is specifically suitable for this: lie on your back and pull your knees towards your chest and stretch them out again. Repeat this 10 times and then take a short break. We advise you to repeat this four times in total.
- Drink a lot! This is probably the most common answer to the question of what helps against constipation. If the intestinal contents are very solid and only move forward slowly, more fluid can help. At least 2 litres of water should be consumed daily.
Medicine-based treatment
If the above measures do not help sufficiently, laxatives (e.g., Glauber's salt, Epsom salts, lactulose or senna leaves, aloe bark, castor oil, bisacodyl, sodium poicosulphate) can be used in the short term under medical supervision. However, caution is advised here, and it is important to consider the side effects of long-term use, such as cardiac arrhythmia due to excessive potassium loss. A potassium deficiency - often caused by laxative abuse - can aggravate the symptoms of constipation. Prokinetics promote intestinal movement (intestinal motility). In this way, food residues are "disposed of" and excreted more quickly. Watch out for side effects!
