Dr. Verena Stieglbauer & Dr. Lukas Grumet
The miracle of the intestines
Our intestine isn’t only our largest organ, with a surface of about 300 square meters, but also offers an important habitat for numerous microorganisms. Discover fascinating details and facts about this organ and how its importance is often and unfairly underappreciated here.
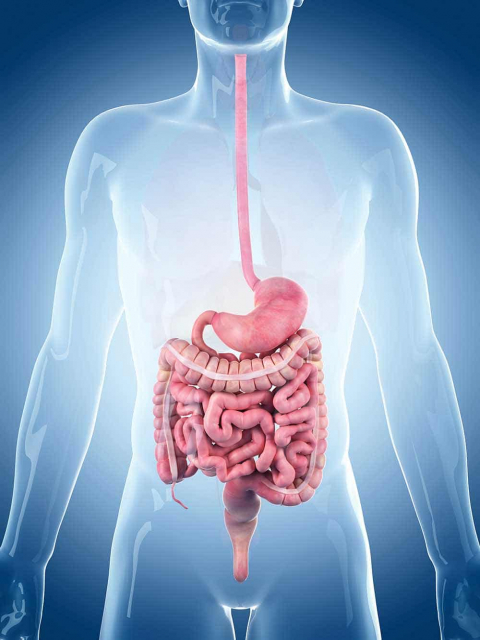
A short introduction into the anatomy of the intestine
The intestine follows the exit of the stomach and is, simply put, made up of 2 main parts: the small and large intestine. The former is subdivided into the duodenum, jejunum and ileum. Let’s start our journey from the stomach downwards: the duodenum first mixes its own digestive juices with the food pulp from the stomach and therefore starts the actual process of absorbing nutrients into our body. Our small intestine breaks the pre-digested food down into its individual parts (for example, amino acids and free fatty acids) and then transports these compounds via the intestinal mucosa into our bloodstream.
The opening between the small intestine and the large intestine is sealed by the so-called Bauhin’s Valve, which prevents the intestinal contents from returning into the small intestine. The large intestine is subdivided into the caecum with the connected appendix, the colon and the rectum. Here, water is removed from intestinal contents to thicken the stool. The bacteria in the large intestine ferment the fibres in our food which the cells use as nutrients and therefore support the function of the intestines.
When looking under the microscope, the structure of the intestinal wall follows the same pattern throughout all sections of our intestines: The intestinal mucosa is the innermost layer of the gut wall. It forms intestinal villi (these are small, frayed-like structures that are responsible for the huge surface area of the gut) which are only found in the small intestine and so-called crypts (these are the protrusions and inversions in the intestinal wall) that are typical for the large intestinal mucosa. The mucosa itself is made up of several thin layers. Below the mucosa lies the submucosa, a layer of connective tissue containing nerve branches as well as delicate blood and lymph vessels. The muscular layer of the gut wall contains transverse and longitudinal muscle fibres so that the intestines can contract in both directions and therefore transport the bolus of digested food along the digestive tract. The outermost layer of the intestinal wall is also a sheet of connective tissue and is known as the serosa.
If we take a closer look at the duodenum, we see a smooth inner surface which is enlarged step by step by folds, villi, crypts and the brush border or microvilli (these are the small protrusions on the surface of the intestinal cells). This surface augmentation is vital for the increased absorption of nutrients and water.
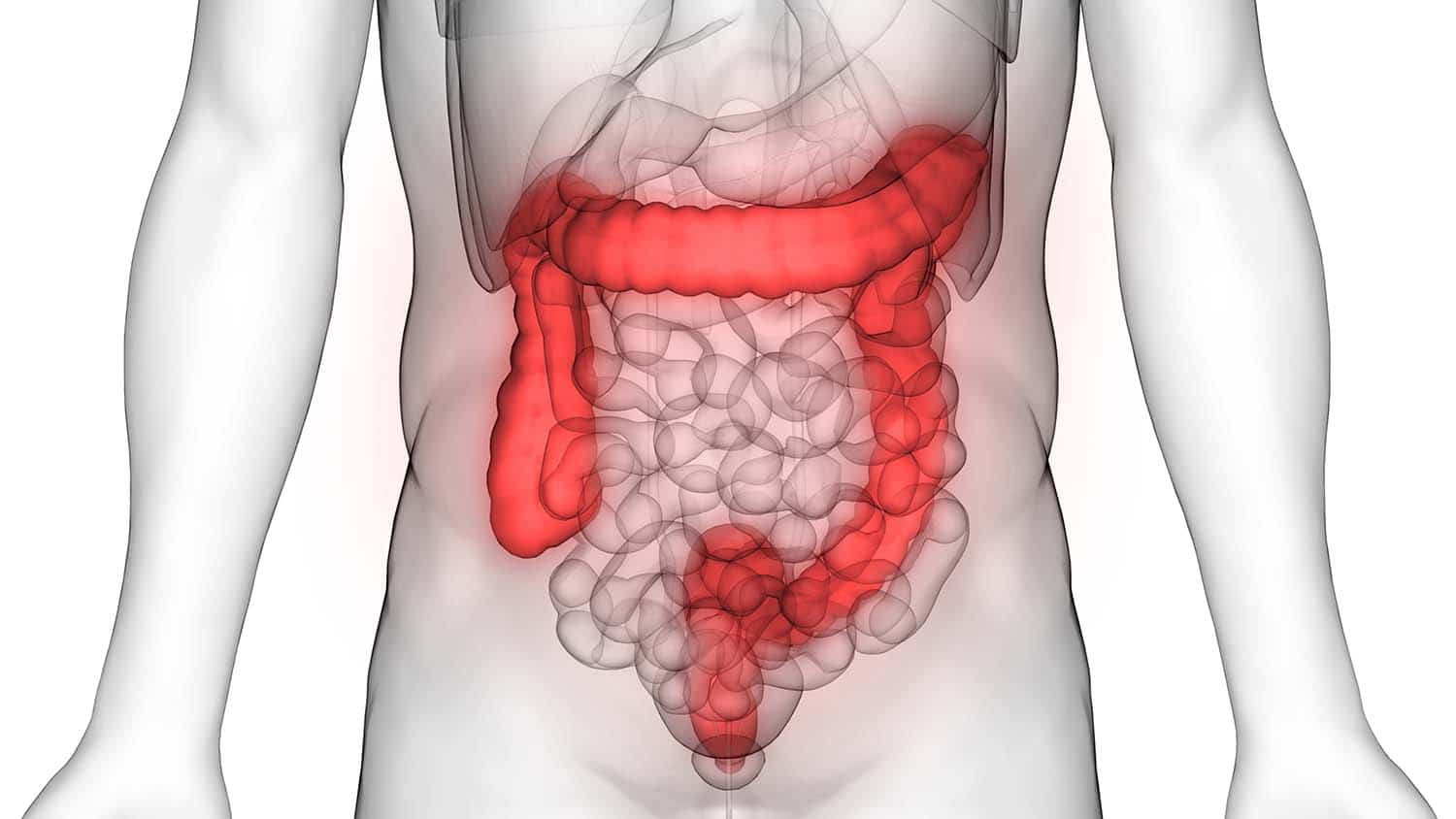
What effect does the microbiome have on intestinal diseases?
The entire digestive tract offers a huge surface for the exchange of metabolised nutrients between microorganisms and human epithelial cells. Depending on the metabolism and the resulting nutrients, the various segments of the digestive tract are inhabited by different bacteria.
The microbiome is responsible for many essential processes in the human body such as the protection from pathogenic agents and strengthening the immune system. A so-called dysbiosis is associated with many different conditions including, among others, chronic inflammatory bowel diseases: Studies show that patients affected by Crohn’s disease have an altered microbiome as well as a lower bacterial diversity in comparison with a healthy person. Even ulcerative colitis shows such a severe altered microbiome composition where fewer short-chained fatty acids, such as butyrate and propionate, are produced. As a result, the activation of immune cells isn’t sufficiently suppressed and thus leads to an increased immune system and inflammatory reaction.
Nowadays, we can effectively treat a dysfunctional microbiome: With the help of probiotics, we can supply targeted bacteria cultures with special abilities. Probiotics whose composition fulfils a certain purpose and whose positive effect has been proven by recognised, scientific studies are especially effective.
Where do they live exactly?
Strictly speaking, the gut of a healthy adult is home to about 100 trillion bacteria (that’s 100.000.000.000.000 living organisms!). Interestingly, this colossal number is only comprised of 500-1000 different types of bacteria, all of which can be assigned to 4 different fractions or „phyla“: Firmicutes, Bacteroides, Proteobacteria and Actinobacteria. Over 99% of these small microscopic inhabitants are anaerobic, which means they need an oxygen-free surrounding in order to survive. This may sound surprising at first, but makes sense when we take a closer look: the human intestine is dozens of meters long and contains, de facto, no oxygen on the inside. And just like humans, bacteria are masters at adapting and know exactly where their optimal surroundings are to survive.
But where do the bacteria actually live? As previously mentioned, the biochemical parameters differ throughout the intestines – from the stomach until the rectum. We, therefore, find different bacteria families along the different intestinal segments.
The small intestine
home of the Lactobacillus Acidophilus

Although the small intestine only contains a small portion of all the bacteria in the intestinal flora (over 90% live a little further „downstream“ in the large intestine), probably the most „popular“ representative with an equally important function can be found here: Lactobacilli such as Lactobacillus Acidophilus stabilise the pH-value by producing lactic acid. If the pH-value in the small intestine were to shift, it could lead to an outbreak of pathogenic agents (such as intestinal yeast). A further function of many lactobacilli is to convert tryptophan molecules into immunologically effective particles. These small lactic acid bacteria play a fundamental role in a functional immune system – and a suppression of such (provoked through a salty, convenience food dominated nutrition) has severe implications.
The large intestine
the Big Apple of microbes

The large intestine is literally a small bioreactor. Here, millions of bacteria ferment fibres into essential micronutrients. Of the many inhabiting florae in the colon, the Bifidobacterium Bifidum is one of the most prominent. This non-motile (=local resident) bacteria belongs to the all-rounders of the intestinal flora in a healthy adult. High-quality studies prove the role that Bifidobacteria play in preventing irritable and inflammatory bowel syndromes. Furthermore, they also stabilise cholesterol levels, alleviate allergic symptoms, improve skin appearance, reduce stress, protect from free radicals – and could possibly play a role in the development of colon cancer. Bifidobacterium Bifidum along with other important probiotic, colon-associated germs such as Bifidobacterium Breve, Lactobacillus Brevis, Enterococcus Durans or Lactobacillus Rhamnosus belong to the so-called „chief bacterial strains“. In other words, they are essential in creating a healthy and functional gut flora and also make sure that numerous other germs can propagate in the intestines.
The intestine: a reservoir of bacteria
A lesser-known, ambivalent role that our gut flora plays is maintaining our sexual health: Studies show that the rectum is a reservoir of naturally occurring vaginal bacteria. According to highly rated studies, if the species Lactobacillus crispatus and Lactobacillus Jensenii were found in the vagina and rectum of female patients, they had a significantly lower risk of developing a bacterial vaginosis than that of patients where both germs were only found in the vagina. At the moment, we assume that this phenomenon is based on the chemotactic migration from the rectum to the vagina, which supports the theory that excessive and aggressive hygienic practices can have a negative effect on the vaginal flora.
Equally exciting is the fact that breastfeeding mothers can transmit their intestinal flora via breastmilk to their children. This mechanism is attributed to the so-called dendritic cells, special immune cells that are able to „catch“ bacteria and travel via our lymph ducts. Dendritic cells can enter the mother’s mammary glands and make sure that the infant is colonised by the mother’s intestinal flora.
The gut as a health centre
Being the home of about 2kg of bacteria, the intestine is probably the most diverse organ in the human body thanks to millions of biochemical exchanges, and we are only beginning to understand the huge importance it plays for our health. The majority of the immune system is produced in the gut. This is where allergies and susceptibility to infections begin. Even chronic diseases such as Parkinson and Alzheimer originate from the intestines. Recent studies even prove that the intestines (including the flora) and the brain are in close contact, and by modifying the intestinal flora through probiotics, we can improve brain function and decision making. The intestines are so much more than a „digestive tube“: Thanks to its diverse gut bacteria, it plays a central role in our health and should be treated as such.