Assoz. Prof. Dr. med. Vanessa Stadlbauer-Köllner
Is the gut flora making our liver sick?
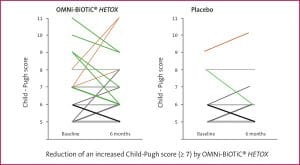
Improvement of liver function during administration of OMNi-BiOTiC® HETOX shown with a reduction of an increased Child-Pugh score (green line).
The study’s most important finding: The improvement of the patients’ liver function was especially significant when the disease was already at an advanced stage. Moreover, the evaluated laboratory parameters showed a significant strengthening of the innate immune system. Fittingly, less study participants in the group receiving the probiotic suffered from infections. We also asked the patients if their quality of life had changed in any way. Encouragingly, we found that the probiotic led to an improvement in life quality.
In conclusion, with this study we were able to show that probiotics provide a good opportunity to improve liver function, immune function, and quality of life in people suffering from liver cirrhosis by positively influencing the gut flora.
*Assoz. Prof. Dr. med. Vanessa Stadlbauer-Köllner, Fachärztin für Innere Medizin, Gastroenterologie und Hepatologie, Leiterin der Forschungseinheit „Transplantation Research“, Medizinische Universität Graz
Liver diseases
Every 370th person suffers from liver cirrhosis. In many developed countries, the disease has become one of the top ten most common causes of death. Many don’t even know they have liver cirrhosis as the symptoms are oftentimes unspecific (for example tiredness, reduced performance, and lack of appetite). Patients with liver cirrhosis often die from complications such as hepatic coma, kidney failure, bleeding, or liver cancer. Liver cancer almost always develops due to pre-existing liver cirrhosis and can only be healed if detected early.
Alcohol, obesity, and chronic viral hepatitis are the most common causes of liver cirrhosis. Men are affected twice as often as women. Patients with liver cirrhosis must get a medical examination at least every 6 months. The exam should include a blood test and a sonogram. The latter is essential to detect liver cancer at an early stage. If the liver cirrhosis is already at an advanced stage then only a liver transplant can help. However, due to the scarcity of suitable donor organs not every patient with liver cirrhosis will be able to receive a transplant.
What is good for the liver – what can harm it?
The liver is an organ which is essential for the body’s metabolism and detoxification. Everything that we ingest, be it food, pharmaceuticals, or toxic substances like alcohol, must by broken down by the liver. Detox therapies with plant-based remedies can oftentimes cause more harm than benefit. This is because plant-based products oftentimes contain high amounts of a certain active substance which may be converted into even more toxic breakdown products in the liver. When a liver has already been harmed it is best to burden it as little as possible.
To avoid:
- Alcohol and its breakdown products damage the gut flora, the intestinal barrier, and the liver itself.
- Fatty and sugar-rich foods increase the gut’s permeability and lead to a fatty degeneration and inflammation of the liver.
- Many pharmaceuticals are broken down in the liver and should therefore be used with caution (e.g. antibiotics and painkillers).
- Plant-based remedies and dietary supplements also contain active substances and therefore should also been taken with caution.
Good for the liver:
- A diverse nutrition helps to keep the gut flora healthy which in turn keeps the gut-liver axis healthy. Unbalanced diets limit bacterial diversity.
- Endurance sport leads to a reversal of the fatty liver degeneration.
- Coffee can improve liver parameters and may possibly prevent the development of scar tissue in the liver.
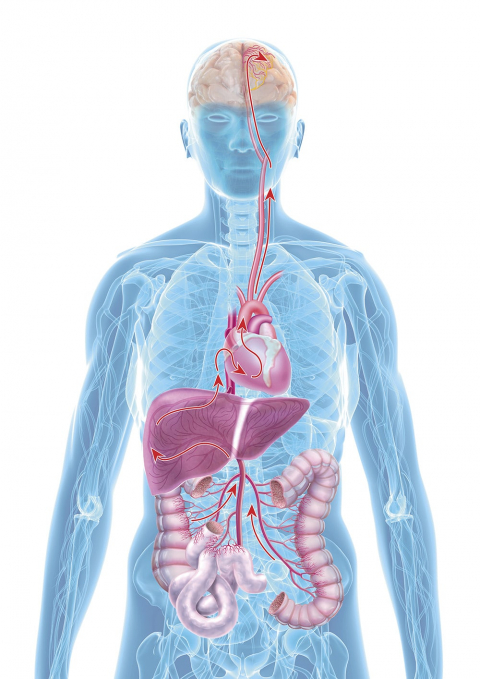
A close relationship between the gut and liver: All nutrients (and toxic substances) which are absorbed by the gut during the digestive process go straight to the liver via the portal vein. Once there, depending on demand, the absorbed nutrients can either be utilised directly, converted, or stored. Toxic substances are broken down before they are released into our circulation and can only then reach the rest of the body.