Claudia Waidacher, MSc. & Susanne ROBERT, MSc.
Bacteria: Superheroes in our Guts!
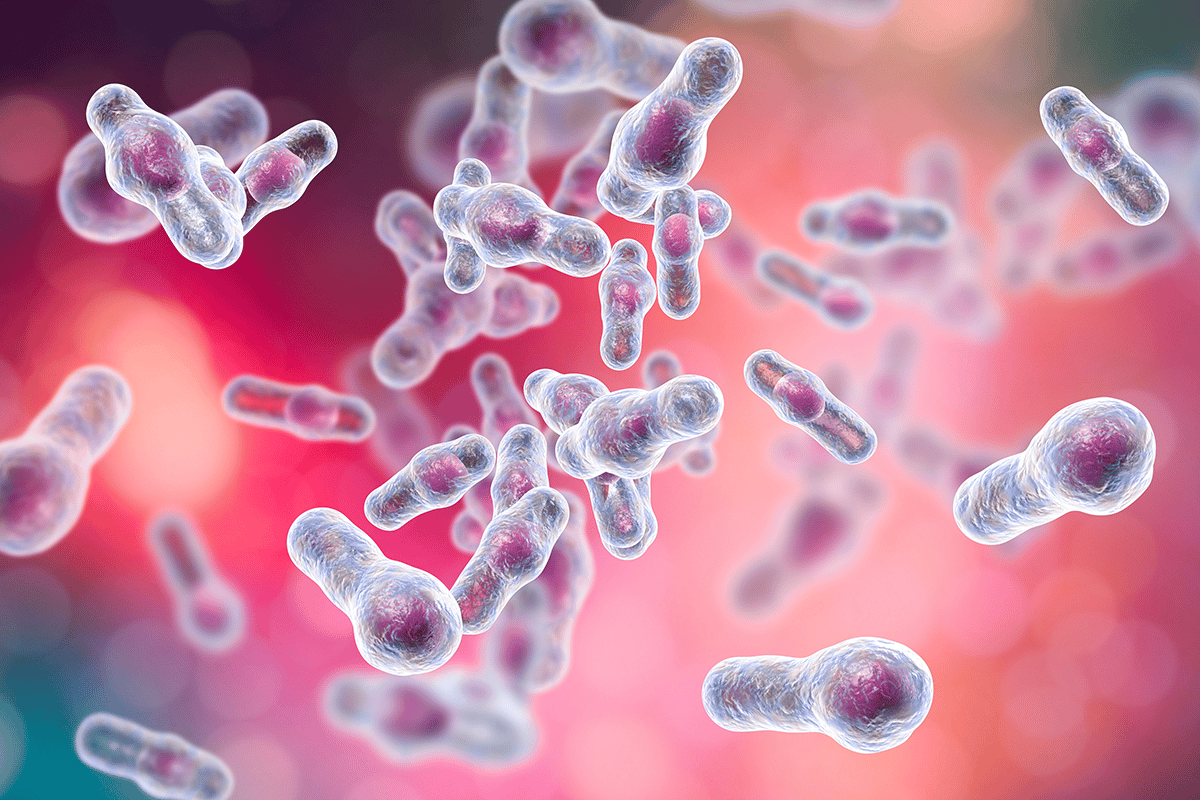
You have probably heard that the gut is the centre of health. But have you ever wondered where this claim comes from? The reason is because of its enormous surface area – the intestine is about 7 metres long and can reach a surface area of about 400 m² (which is about the size of a tennis court), and the intestine must be ready to fight and repel possible intruders. This defence force is formed by several mechanisms. On the one hand, about 80% of our immune cells are located in the intestinal tissue to fight invading bacteria or viruses, and on the other hand, a large number of microorganisms also live in our intestines. These microorganisms also play their part in choosing us as their habitat. Our intestinal bacteria are in fact able to displace and repel pathogenic bacteria and viruses through various mechanisms.
Our intestinal microbiome has a very complex structure. Around 500 different species of bacteria colonise the different sections of a person’s intestine and also bring enormous positive effects for the host – as long as it is a eubiotic, i.e. a healthy intestinal microbiome and no pathogenic bacteria have made themselves at home. The gut microbiome can contribute to strengthening the health of our gut and the rest of our body in several ways. Very general positive effects include strengthening the gut barrier. Some gut bacteria are able to boost the production of mucus in the gut. The intestinal mucus forms an important barrier against invading microorganisms and also contains, among other things, antiviral or antibacterial substances, such as secretory immunoglobulin A, an antibody that can attach to harmful organisms and make them visible to our immune system (think of it as a marker by which we can recognise bad guys). In addition to increasing mucus production, good gut bacteria can also attach to and occupy receptors on our gut wall. This means that these sites are no longer freely accessible to other, harmful viruses or bacteria, which are then also unable to penetrate the body and cause damage.
Gut bacteria: Which are the good types?
Different types of bacteria and especially strains of bacteria are also capable of even more specialised defence mechanisms. Through these mechanisms, they can specifically act against invading viruses, for example, and destroy them or prevent them from entering our body cells. Through so-called “trapping”, bacteria can catch and hold viruses on their surface. This happens via longer sugar chains, so-called polysaccharide chains, to which the virus is held. As a result, it is no longer able to continue on its way to the intestinal cells and enter the body. Other bacteria are able to release special antiviral substances from their interior. These include very small molecules such as hydrogen peroxide (H2O2) or lactic acid (lactate), but also larger amino acid compounds (peptides) called bacteriocins. These substances can prevent replication, i.e. the reproduction of viruses in a cell. Thus, the virus cannot replicate, infect new cells and spread further. In addition, bacteria have another ability: they can enter into direct contact and exchange information with our immune system. This can happen, for example, via the dendritic cells in our intestines. Dendritic cells are star-shaped immune cells that patrol our body. With their extensions, they can reach through our intestinal wall and control the position in our intestinal lumen. In doing so, they come into contact with our gut microbiome. Depending on which bacteria they communicate with, they receive different signals and information that they pass on to other cells of our immune system. In this way, a modulation of the immune system can occur and our immune cells are alerted, which increases the defence power.
Probiotics: Special strains of bacteria to fight viral infections
In many studies, the administration of probiotics, or good intestinal bacteria, during viral infections has been shown to have many positive effects. Certain bacterial strains have proven to be specialists in this field: For example, the bacterial strain Lactobacillus rhamnosus SP1 was shown to reduce the frequency, duration and severity of diarrhoea during rotavirus infections (Pant et al. 2007). Furthermore, ingestion via the gastrointestinal tract contributes to the alleviation of symptoms of influenza A infection and to a lower viral load in lung tissue (Kawase et al. 2010). But not only the acute therapy of already existing infections brings positive effects. Preventive administration can also bring surprising results to light, as in the study by Villena et al. (2012). Here, the administration of Lactobacillus rhamnosus CRL 1505 reduced lesions in the lung tissue and regulated the production of antiviral cytokines. This means that there was less damage to the lung tissue during a viral infection due to the preventive ingestion of the bacterium.
B. animalis ssp. lactis DSM 15954 is also a pro in viral defence. Administration resulted in a significant reduction in respiratory tract infections in healthy newborns (Taipale et al. 2011). Specially matched bacterial teams can also lead to particular improvements as a double pack. The combined administration of Lactobacillus rhamnosus SP1 and Bifidobacterium animalis ssp. lactis DSM 15954 was able to significantly reduce the duration of upper respiratory tract infections, the severity as well as the number of missed school days in students (Smith et al. 2013). These results show the amazing abilities our good gut inhabitants are equipped with and put to work for us and our health. You may have wondered if gut bacteria are even capable of fighting viruses outside our gut, even in other parts of the body. This question is justified. But as has been shown in many other areas, the gut is linked to the rest of our body via various axes. The gut-brain axis or the gut-liver axis are well known examples that show that our gut microbiome has a great influence on our health and can influence it positively. Another axis that is still little known is the so-called gut-lung axis.
Gut-Lungs Axis
Studies such as those mentioned above clearly show a positive effect of our intestinal bacteria on lung infections, thus clearly demonstrating that there is an exchange between our intestines and our lungs. This exchange takes place via our immune cells. As mentioned, intestinal bacteria are able to exchange information with our immune cells. This information, which is passed on to cells of the immune system, leads, among other things, to an increase in natural killer cells and to increased macrophage activity in the lungs. These cell types are particularly responsible for the rapid destruction of invaders and thus prevent viruses from spreading far into the lung tissue and multiplying