Ageing with a healthy gut
Humanity’s dream of eternal life on earth will never become a reality. Science estimates that the oldest people will ever get is around 120 years. This corresponds with the age of the world’s oldest person on record: The French woman Jeanne Calment died at the age of 122 years and 164 days in 1997. From the perspective of modern medicine, it’s not the number of years that count. Instead, what counts is the state of health people are in when they reach an advanced age. The exact timepoint when the natural aging process begins in humans isn’t easily defined. However, physicians and age researchers alike can agree that starting with one’s 35th year of life, aging starts to speed up (see info box). What happens? How does it happen? And why does it begin in exactly those years? These questions remain largely unsolved, which in turn provides a lot of material for many future research projects. Generally, it can be assumed that a combination of genetic predispositions (e.g. in regard to cell ageing), environmental influences, social factors, as well as epigenetic alterations influence aging during the course of one’s life.
Dementia – the scourge of the elderly
An issue which has been puzzling many in the field of medical research is the “scourge of the elderly”: Forgetfulness, dementia. We are still waiting for a major breakthrough when it comes to a therapy for these diseases. What modern medicine knows so far is that there are preventative measures with which we can make sure the disease never emerges. Some examples for such preventative measures would include activities such as playing board games, reading, learning a new language, or dancing. Moreover, more and more scientific literature is being published which indicate that the gut flora (the microbiome) has an influence on the psychological deterioration which occurs in the course of dementia. Austrian physicians such as Professor Friedrich Leblhuber are at the forefront of international research in this field.
Leblhuber works as a specialist physician for neurology and psychiatry in Linz (Austria) and his area of expertise concerns neuropathological processes. “The developments in microbiome research have been fascinating”, says Leblhuber and by this he means, amongst others, the results of a scientific study which was published in the renowned scientific journal “Neural Transmission”. In this collaborative work between the state psychiatric clinic of Linz, the Medical University of Innsbruck (Austria), and the Biovis Institute in Limburg (Germany), inflammatory markers were measured in patients suffering from dementia.
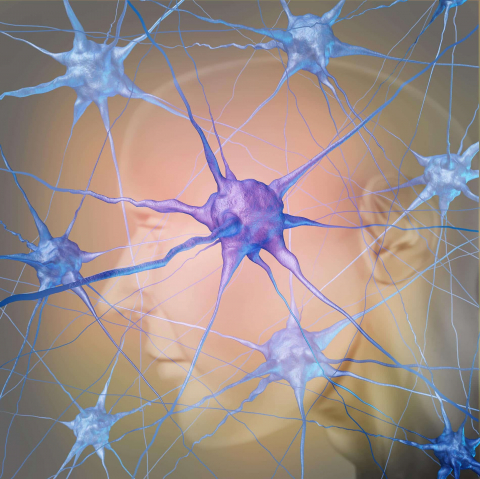
Our brain can suffer damage due to inflammation of nerve tissue, leading to diseases such as dementia and others.
Uncovering “silent” inflammation
But how? Highly specialised laboratory methods and gene technological procedures make this possible, for example through the analysis of patient’s stool samples. In this way, so-called inflammatory markers can be identified. They provide information whether inflammatory, yet asymptomatic, processes are taking place in a patient’s body and if so how severe they are. Leblhuber and his colleagues examined these markers in patients suffering from dementia. They did this because many findings indicate that there is a correlation between inflammatory and degenerative processes in the brain. “Our findings, which were met with a high degree of interest by the scientific community, show that inflammatory markers in the stool show a significant inverse correlation with low tryptophan, tyrosine, and phenylalanine levels in serum samples”, explains the neurologist. “A follow-up study with 43 Alzheimer’s patients showed similar results: Alpha-1-antitrypsine and calprotectin, both parameters which point towards an inflammatory process, were significantly increased. At the same time, it was shown that in all these cases there was a lower number of the anti-inflammatory bacterium Faecalibacterium prausnitzii in the gut of the patients.”
An armada of specific immune cells like leukocytes and lymphocytes is sent out to defend the body against viruses and other germs.

Inflammation of the gut weakens the gut’s barrier function. This means that harmful substances can enter the bloodstream. Inflammatory cells can penetrate virtually any region of the body.
Harmful substances from the gut
All this sound awfully complicated and ultimately, it is. However, medicine has known the significance of “silent” inflammation in the development of diseases for quite some time now. In the year 1999, it was shown that a blood clot, which leads to the blockage of a coronary artery and subsequently a heart attack, contains the same inflammatory substances which occur in a joint affected by rheumatoid arthritis. Research projects in the last ten years have brought yet another factor into the fray: The damaged, leaky gut with an altered gut flora and its effects on the gut-brain axis. A leaky gut means a dysfunctional gut barrier. If the gut mucosa becomes permeable this means that harmful substances can enter the entire organism via the bloodstream; even the central nervous system (CNS) and thereby the brain. The term “leaky gut” was coined as early as the 1990s when it was used in a scientific publication. Back then it was mainly used in complementary and alternative medicine. However, this is definitely no longer the case. Nowadays experts in conventional medicine consider it very much possible that many diseases such as obesity, dementia, coeliac disease, and even liver damage may be associated with an impaired gut barrier.
Inflammation alters the brain
If spread out, the guts inner surface area would cover an area of over 400 square metres. It not only regulates the absorption of nutrients, it also keeps potential harmful substances from entering the body. The functioning of these mechanisms seems to be dependent on “binding substances” between the gut epithelial cells, the so-called “tight junctions”. If there are disruptions in the immune system’s complicated signal pathways, then harmful substances are no longer recognised and the body’s defence processes fail. The gut becomes permeable, namely for substances which shouldn’t be able to enter the body with our food’s nutrients: Noxious germs, toxins, or allergens. Alterations of the gut flora play an important role when it comes to the development of such pathological processes.
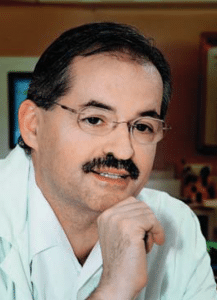
Professor Friedrich Leblhuber, specialist for neurology and psychiatry in Linz
Leblhuber explains which possible implications a immunodeficiency may have on the central nervous system: “A leaky gut develops due to regional inflammatory processes. A passing over of inflammatory cells into the bloodstream leads to additional chronic inflammation of other peripheral body regions. Finally, the inflammation cascade leads to neuroinflammation via the autonomous nervous system. This is what leads to the early changes in the brain which can be seen in patients suffering from Alzheimer’s dementia. This process may begin decades before the onset of any symptoms. Ultimately, the starting point of all this is a leaky gut which we can detect by analysing a patient’s stool for specific markers such as Calprotectin. A Swedish research team clearly postulated that, judging by their studies, the development of Alzheimer’s disease and other neurodegenerative diseases originates from the microbiome.”
Probiotic intervention
Leblhuber also thinks it’s plausible that a therapy with specific anti-inflammatory probiotic bacteria can influence inflammatory processes. In the meantime, there are even results to back this up: Animal and clinical experiments confirm that the administration of a probiotic reduces inflammatory processes in the gut. Because alterations of the microbiome and damage caused by inflammation occur relatively early in the course of neurodegenerative diseases like Alzheimer’s, it may be beneficial to start a probiotic therapy as early as possible. This theory is becoming widely accepted by experts around the world. At the moment, other studies are being conducted to further elucidate the highly complex processes which are at play here. “If it should ever be possible to completely stop regional inflammation in the gut, say with the help of probiotics, then this should delay the degenerative processes in the brain which ultimately lead to Alzheimer’s dementia”, says Leblhuber.
How humans age
Ageing is a natural process which spans over the course of decades. It affects the entire body and all its organs. At the same time, there are big differences regarding the degree to which aging affects specific organs and the timepoint when the first signs of aging occur. Listed below are several of the most significant age-related changes:
Eyes: The eyes ability to adjust to close objects is reduced (presbyopia), as well as the eye’s adaptability in changing light conditions. These deterioration processes mostly begin around the age of 40.
Hearing: A deterioration of hearing capacity – concerning the volume that is necessary to hear something, the comprehensible sound frequencies, and the comprehension of speech – mostly results from age-related damage to the inner ear. Hearing bothersome noises (tinnitus) is also oftentimes age-related.
Smell, taste, and thirst: A successive decline in the ability to differentiate between smells and distinct flavours. For this reason, old age can result in a loss of appetite and thus an unbalanced diet. The sensation of thirst becomes less pronounced, which is why the elderly often drink too little.
Bones: Bone quality is dependent on a balanced forming and resorbing of bone tissue. With increasing age resorption outweighs the forming of new bone tissue, especially when someone is also suffering from a vitamin D deficiency. Regular physical exercise can slow down this process significantly.
 Brain: The number of brain cells constantly declines, the signal transmission between the nerve cells decreases or is lost completely. Additionally, the layer which acts as isolation for nerve cells is consecutively removed with advancing age. This leads to a decline in one’s reaction speeds and processing abilities. However, the brain is trainable all the way into old age. The functions of degraded or malfunctioning nerve connections can be taken over by other nerves, or new brain cells can even be formed.
Brain: The number of brain cells constantly declines, the signal transmission between the nerve cells decreases or is lost completely. Additionally, the layer which acts as isolation for nerve cells is consecutively removed with advancing age. This leads to a decline in one’s reaction speeds and processing abilities. However, the brain is trainable all the way into old age. The functions of degraded or malfunctioning nerve connections can be taken over by other nerves, or new brain cells can even be formed.
The skin becomes thinner and dryer. It loses its protein fibres, such as collagen, which make it elastic and stretchy. Its water storage capacity decreases and the subcutaneous fat tissue is depleted.
Muscles build up far slower than in one’s younger years. Fat deposits begin replacing the muscle mass which is lost. Targeted training slows down this process. Strictly speaking, it’s even possible to increase one’s muscle strength at an advanced age.
Heart and circulation: The heart is also a muscle. During the aging process muscle cells are replaced with connective tissue, which leads to decreased cardiac performance.
The immune system produces less and less immune cells and antibodies. The susceptibility to infection increases. Once trivial diseases suddenly become more serious with age; complications occur more often. This is also due to the fact that age-related damage to the gut has a negative effect on the immune system. After all, 80% percent of the body’s immune system is located in the gut.
Gut and digestion: With old age the body’s glands begin to slow down the production of hormones and digestive juices. Furthermore, eating habits change and oftentimes a permanent intake of medications is also necessary. All these factors lead to changes in the composition of the gut flora: The number of useful lactobacilli and bifidobacilli decreases. They are replaced by putrid bacteria which have a negative effect on the digestive process.